FSH: Follicle-Stimulating Hormone is a glycoprotein, which, like LH, hCG and TSH consists of alpha and beta chains. The alpha chain is virtually identical in all four hormones, whereas the beta chains are different and determine both the specific biological activity and immunological characteristics of each hormone. The FSH molecule contains approximately 16% carbohydrate and has a molecular weight of approximately 28,000 to 30,000 daltons FSH stimulates ovarian follicle growth and estrogen production in women, and testicular spermatogenesis in men.
Hypothalamic control of FSH secretion by the anterior pituitary is done by gonadotropin-releasing hormone (GnRH) with negative feedback at the hypothalamic level by estrogen in the female and testosterone in the male.
Determination of FSH concentrations is essential in assessment and monitoring of patients with suspected infertility.
LH: Human Luteinizing Hormone is a glycoprotein, which, like FSH, HCG and TSH consists of alpha and beta chains. The Alpha chain is virtually identical in all four hormones, whereas the beta chains are different and determine both the specific biological activity and immunological characteristics of each hormone.
The LH molecule contains 15-18% carbohydrate and has a molecular weight of approximately 29,000 daltons. LH induces ovulation and thereafter maintains the corpus luteum and progesterone production in women. In men, LH stimulates testosterone production by the Leydig cells.
Hypothalamic control of both LH secretion by the anterior pituitary is done by gonadotropin-releasing hormone (GnRH) with negative feedback at the hypothalamic level by estrogen in female and testosterone in male.
Determination of LH concentrations is critically important in assessment and monitoring of patients with suspected infertility. The raised levels of LH and LH: FSH ratio is frequently found in polycystic ovary syndrome (PCOS), a common cause of infertility in women.
HCG: Human chorionic gonadotropin is a glycoprotein, which, like LH, FSH and TSH consists of alpha and beta chains. HCG is produced by the placenta shortly after implantation and increases at a geometric rate until it reaches a peak near the end of the first trimester. This makes it an excellent marker for the confirmation of pregnancy and/or monitoring its course thereafter when necessary.
This hormone is produced by the pituitary gland, and its primary function is to stimulate milk production. But prolactin also affects ovulation and menstruation, and too much prolactin in the blood can cause infertility by inhibiting FSH and GnRH (gonadotropin releasing hormone), and blocking ovulation from being triggered.
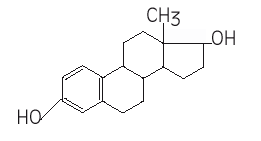
Estradiol-17β (E2), a steroid hormone with molecular weight of 272.4, is the most active estrogen in the body. It is produced in woman by the ovarian follicles, corpus luteum, placenta and adrenals. In men small amounts are produced by the testis and due to peripheral conversion of testosterone.
Physiological Action in Women
E2 is a real feminization hormone. At puberty, E2 promotes the development of the female secondary sexual characteristics, like the growth of the uterus, the vaginal mucous membrane and the development of the mammary ductal system.
In non-pregnant subjects there is cyclic variation in the concentration of E2 with the highest concentrations occurring just prior to ovulation. In the first half of the menstrual cycle, follicle stimulating hormone (FSH) accelerates follicular development and E2 secretion. Rapid secretion of E2 imposes a positive feedback influence upon the pituitary gland, resulting in the release of luteinizing hormone (LH) from the pituitary, and ovulation begins. E2 direct the metabolism toward the storage of fat and also promotes the absorption of calcium in the bones.
Physiological Action in men
Role of circulating E2 in male reproductive health appears to be insignificant
Clinical utility of E2 measurements in women
The measurement of E2 simultaneously with FSH and LH levels can provide information to diagnose fertility problems:
1. Assessment of the ovarian function
2. Monitor of the hormonal infertility treatment and follow up of IVF
3. Differential diagnosis of amenorrhea
Amenorrhea is defined as the absence of menstruation for 3 or more months in women with past menses.
4. Evaluation of precocious puberty for girls is the appearance of secondary sexual development earlier than the mean. The new guidelines propose that precocious puberty be defined by the presence of breast or pubic hair development before age 6 years in African-American girls and age 7 years in Caucasian girls
5. High levels can be an indication of ovarian neoplasm
Clinical utility of E2 measurements in men
1. Gynecomastia, breast development in males, is affected by the same hormones that stimulate female breast growth tissue. As the testes secrete only small amounts of estradiol the remainder of estrogen in males which is the cause of Gynecomastia, is derived from the extra glandular aromatization of testosterone and androstenedione to estradiol and estrone.
2. Feminization
3. Hypogonadism
4. Testicular tumors can lead to increased blood estrogen levels by: estrogen overproduction or by androgen overproduction in combination with aromatization in the periphery to estrogens. Although the testicular tumors with overproduction of estrogens are rare, they can be the cause of gynecoimastia. Note theses tumors are coming from Sertoli cells or granulose cells in the testis? Tumors derived from germ cells are producing HCG.
Progesterone is produced in females mainly by the ovaries (corpus luteum) small amounts are produced by the adrenal and during pregnancy by the placenta. The main function is to regulate the condition of the endometrium of the uterus.
Progesterone has also effects on other female organs.
DHEA-S: Dehydroepiandrosterone sulfate is a steroid hormone, secreted from adrenal cortex. DHEA-S level in the blood, are higher in men as in women by all age groups. And both in men as in women DHEA-S decrease gradually after a peak of 20-years old time.
Dehydroepiandrosterone sulfate (DHEA-S) is secreted by the adrenal cortex in response to adrenocorticotropin (ACTH). Small amounts are also produced by the ovaries and testes.
DHEA-S is an androgen (MW 371), a male sex hormone, which is present in the blood of both men and women. It has a role to play in developing male secondary sexual characteristics at puberty, and it can be metabolized by the body into more potent androgens, such as testosterone and androstenedione, or can be changed into the female hormone estrogen.
Since DHEA-S is primarily produced by the adrenal cortex , it is useful as a marker for adrenal function in combination with testosterone and other androgens. DHEAS can be measured to help diagnose adrenal tumors, cancers, and hyperplasia and to separate these conditions from ovarian tumors and cancers. Concentrations of DHEA-S are often measured, along with other hormones such as FSH, LH, prolactin, E2 and testosterone, to diagnose polycystic ovarian syndrome and determined the cause of infertility, amenorrhea and hirsutism. DHEA-S is anso used, along with other hormones, to investigate and diagnose the cause of virilization in young girls and precocious puberty in young boys.
SHBG: Sex hormone-binding globulin, one of blood transport proteins, is a large homodimeric glycoprotein that especially binds testosterone and estradiol. It is mostly synthesized in the liver and is released into the bloodstream. The biological activities of these sex steroids in plasma are regulated by plasma SHBG, since its high binding affinities to the steroids limit these access to target cells.
It is suggested that SHBG concentrations are influenced by various factors, such as thyroid hormones, estrogens, insulin, and several growth factors. Increases in SHBG levels are found in hyperthyroidism, hepatic cirrhosis, and pregnancy. High SHBG values are also seen with oral estrogen treatment, tamoxifen administration, and Klinefelter’s syndrome. Decreases in SHBG levels are observed in female patients with hirsutism, hyperandrogenism, or insulin resistance syndrome. In hypothrroidism, SHBG are often lowered.
SHBG are widely measured together with testosterone assays to calculate the “Free Androgen Index” (FAI), the ratio of total testosterone level derived by SHBG level. The FAI is known as a useful indicator to determine abnormal androgen status.